 Testicular cancer although a relatively rare cancer (2% of men are affected), is the most commonly occurring cancer in boys and young men between the ages of 20-40, becoming the third leading cause of death at these ages. Currently it is considered to be the most treatable form of urinary tract cancer and the survival rates in its early stages are almost 100%.
Testicular cancer although a relatively rare cancer (2% of men are affected), is the most commonly occurring cancer in boys and young men between the ages of 20-40, becoming the third leading cause of death at these ages. Currently it is considered to be the most treatable form of urinary tract cancer and the survival rates in its early stages are almost 100%.
Epidemiology
In the US and UK the probability of the disease is 1:500 with an increasing trend in recent years. In 78% of cases, testicular cancer occurs between 20-40 years, 20% in men> 40 years and 2% in boys <15 years. White men are affected four times more than blacks. It is more commonly found in the right testicle (like cryptorchidism), for hitherto unknown reasons.
Pathogenesis - Risk factors
In recent years there have been different views on the pathogenesis of the disease, however, its causes remain essentially unknown. Occasionally, several factors have been implicated, congenital or acquired, such as injuries and trauma, repeated infections, the administration of estrogens or antiandrogens to the mother during pregnancy, continuous exposure to various substances (such as phenols, fertilizers, lime, tobacco), inguinal hernia and testicular mikrolithiasis.
The only proven link is the one between cryptorchidism and testicular cancer growth (3 to15 times greater chance of developing cancer in cryptorchidism). Hereditary disposition is found in only 2% of patients and is associated with a mutation in the X chromosome. Moreover, patients with a history of cancer in one testis, exhibit a 2% probability of a second primary tumor appearing on the contralateral testis.
Diagnosis
Painless swelling is the normal clinical manifestation of testicular cancer (one in two patients). The patient usually finds out about the swelling himself or it is discovered by the sexual partner. More rarely (30% of cases), the patient feels heaviness or pain in the scrotum. Reactive hydrocele or inflammation may also be present, a condition that complicates proper diagnosis. It is worth noting that in 30% of the cases, symptoms of metastases from the first examination are prominent, such as pain in the loins from the swelling of the retroperitoneal lymph nodes, coughing and shortness of breath from lung metastases, swelling in the epigastrium from enlarged abdominal lymph nodes (the most common symptom of children's tumors ), pain in the cervical region (due to supraclavicular lymph nodes), nausea, vomiting and weakness. Also 5% of the patients exhibit gynecomastia.
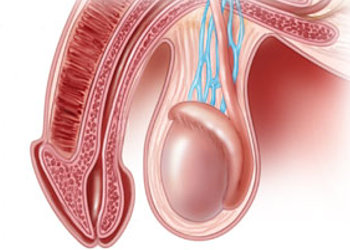
Clinically the testicle is hard, swollen and painless, while other elements of the scrotum (the epididymis and spermatic tone) are normal.
Classification of testicular tumors
Neoplasms of the testes can be distinguished in:
A. Primary tumors from germ cells (95%) composed by two main categories:
1) the seminomas (35% of tumors) and
2) the non-seminomatous tumors (65%) with embryonic carcinoma as the most common type (20%),
teratoma (5%) and gross tumors (40%).
B. Tumors from non-germ cells (5%).
Diagnosis-Laboratory-Radiological assessment
In the diagnosis, the role of laboratory tests is important and it includes:
Biochemical tests on tumor markers (beta-chorionic gonadotropin, alpha-fetoprotein, LDH), which are typically high in certain types of cancer. It should be noted, that the presence of a normal range of the tumor markers, does not exclude the possibility of a cancer diagnosis.
Chest X-ray: The first test for pulmonary metastases.
Scrotum ultrasound: Testicular tumors have a distinctive image.
Intravenous urography: Gives information on any retroperitoneal lymph node swelling.
Computed tomography: Examination of choice in metastases detection.
Bone gammagraphy and CT brain scan: In case of relevant symptoms.
The final diagnosis is made after excision of the testis and its histological examination.
Differential diagnosis
Differential diagnosis is made from all conditions that cause swelling of the scrotum including orchitis, epididymitis, hydrocele, haemocoel, hematoma of the scrotum, spermatocele, twisting of the testicle and epidermoid cyst.
Treatment
Radical orchiectomy with high ligation of the spermatic tone is usually the initial treatment. Further treatment is decided depending on the histological type of the tumor and the presence or absence of metastases. Additional treatments include radiotherapy, chemotherapy and surgical excision of the lymph nodes that are affected. The prognosis is generally very good and this is due to the effectiveness of chemotherapy.