 What is the prostate?
What is the prostate?
It is a gland in the male reproductive system. It has a shape the size of a chestnut. It is located behind the pubic symphysis, directly under the bladder and it surrounds the urethra's initial part. When the prostate becomes enlarged it presses upon the urethra causing disturbances during urination. Its function is related to fertility.
The prostate's secretions along with the ones from the seminal vesicles constitute the major part of the seminal fluid into which the spermatozoa are mixed and is eventually produced by the testes. This exudate provides necessary nutrients and substances for spermatozoa's normal functioning. The prostatic secretion is regulated primarily by the action of androgen hormones and neuronal stimuli.
Prostate Diseases
Benign prostatic hyperplasia (BPH)
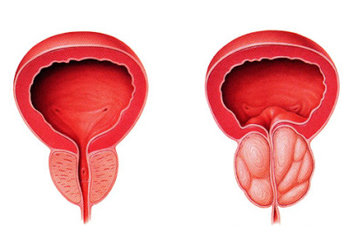
As the man grows older, it is normal for the prostate gland to swell. This expansion happens in the inner part of the gland and it is due to the proliferation of all its cellular elements and is known as benign prostatic hyperplasia (BPH). The etiology of hyperplasia is multifactorial. It is certainly associated with age and the relevant hormonal changes that occur. It is also probably associated with smoking, alcohol consumption, obesity, hypertension and diabetes. The hyperplastic prostatic tissue presses the prostatic part of the urethra that passes through its interior, reducing the lumen's diameter, thus preventing the normal flow of urine.
What are the problems associated with benign prostatic hyperplasia?
The symptoms exhibited by a man with an enlarged prostate include a weak or decreased radius of urination, delay in starting urination, interruptions during urination and a feeling of incomplete emptying of the bladder due to urinary residue that remains after each urination. These symptoms are classified as obstructive and are due to the blockage of the enlarged prostate on the urethra. At the same time, other symptoms also appear that are particularly troublesome including frequent urination throughout the day, nocturia (frequent awakening at night to urinate) and an urgency to urinate (sudden urge to urinate that can not be suspended which several times can lead to urgent urinary incontinence).
Those symptoms that are classified as irritant are due to changes made in the muscular wall of the bladder which is overloaded while trying to overcome the barrier posed by the obstructed urethra. The symptoms are very bothersome and affect the quality of life of male patients. Daily activities and social contacts become limited, frequent awakenings at night affect the quality of sleep, so patients feel tired the next day with a reduced vigor and productivity while eventually their mental and physical health may be affected. In such cases, people may be forced to organize their activities so as to be near a toilet. Certainly, the severity of the symptoms is not the same in all men with benign prostatic hyperplasia and such symptoms can be rated accordingly. They can be broken down into mild, moderate and severe ones.
It is understood that the symptomatic enlargement of the prostate is a disease that primarily affects the quality of life but seldom threatens life. BPH seems to be a slowly progressive disease if left untreated. The prostate grows every year, the flow of urine decreases continuously and urine residue increases. These can lead to complications such as urinary tract infections and stone formation (lithiasis) of the urinary bladder (a result of microbial inflammation of urine remaining in the bladder after each urination), the occurrence of diverticula that constitute a projection of the bladder's mucous membrane through its muscle wall. The diverticula are the result of increased pressure in the bladder during urination.
Other complications are hematuria which usually accompanies the appearance of an enlarged prostate, urine retention and also incontinence due to urine overflow. In this case, the bladder becomes enlarged and retains large quantities of urine. During the day, the patient exhibits very frequent urination while at night urinary incontinence appears. This situation is particularly dangerous because it can cause great dilatation of the ureters and kidneys (obstructive uropathy) and affect kidney function. If the patient neglects it and does not promptly seek the advice of a urologist, the condition may become irreversible and result into chronic renal failure. For this reason, every man showing such symptoms while exhibiting disturbances during urination, should visit a urologist.
The urologist will determine the severity of the symptoms, rate the quality of renal function, urine flow, measure the residual urine in the bladder after urination and examine the patient's prostate by conducting a dactylic rectal examination. Based on the findings of the examination and considering the general state of the patient's health taking into account any other concomitant diseases, the urologist will propose to the patient an appropriate treatment.
What is the treatment of symptomatic BPH?
In patients with mild symptoms that do not affect the quality of life, simple monitoring is usually suggested which includes some lifestyle changes and an examination, usually every 6 months. In patients with more severe symptoms affecting their lives, drug treatment is initially proposed. There are drugs that relax the prostate, thus facilitating urination with a rapid improvement of symptoms and without affecting its size. There are also drugs that shrink the prostate, improving symptoms but at a slower pace. Usually they are given to those patients whose prostate is very large. There may also be a combination of drugs when the doctor deems it necessary. In patients whose symptoms are not relieved by medication or who exhibit any of the above complications of BPH, resorting to surgery may be necessary.
This is usually done by subtracting the prostate adenoma (that part that presses on the urethra), or subtracting it through an open section when the adenoma is too large or by cutting it piece by piece from the urethra, with a special tool. Both methods are very effective and due to the progress of technology and anesthesia, the complications from such surgeries are minimal. It should however be noted that removing that portion of the prostate does not protect the patient from a future occurrence of prostate cancer, this happens because this procedure does not remove the entire prostate, but the portion that presses the upon the urethra.
Patients who are very old and have a high surgical risk because of other coexisting diseases, other methods may be tried which are described as minimally invasive. These include microwave thermotherapy, high-intensity focused ultrasound, radio waves and laser. These processes are generally characterized by a significant reduction in morbidity but without achieving the same effects as prostatectomy and the number required re-operations is significantly high. Recently, two new laser techniques, KTP (green light) and Holmium Laser, seem to be highly effective, enabling the removal of the prostate almost bloodlessy, with a brief hospital stay, rapid removal of the catheter and a significant improvement in urination. There are not yet conclusive results of monitoring patients for a long time, so that such procedures may be recommended unreservedly as the best method of surgical treatment of prostatic hyperplasia.
Prostate Cancer
What is prostate cancer?
In the normal prostate, as in most organs of the body, there is a well-regulated cell growth. As the aged cells die (apoptosis), new cells are being created, with the same function as the old ones. In cancer, this setting is missing and the cells multiply without the usual control, resulting to many genetic errors that accumulate so that cells do not function normally any longer. Thus cancer constitutes an abnormal or unregulated cell growth, and when this happens in the prostate, it usually begins in the outer zone of the gland. This means that a small prostate cancer may be present without causing any symptoms during urination because it does not depress the urethra since urine can easily pass the capsule and come out of the prostate.
Because growth of cancer cells is uncontrollable, the malignant tumor can infiltrate adjacent organs, or even grow in other parts of the body (metastasis)
How common is prostate cancer?
It is the most common cancer in men and the second leading cause of death from neoplastic disease after lung cancer. The histological form (subclinical form) is very common and its incidence rate is similar throughout different races. However, the clinical form (the one that exhibits symptoms) has a lower incidence rate that differs throughout races (more common in blacks) while also exhibiting geographical differences (higher rates in Nordic countries, lesser in the Mediterranean and very low in Asia).
What are the causes of prostate cancer?
Prostate cancer appears to be directly associated with age and hormonal status. This involves genetic factors defined by race and heredity, as well as dietary factors. Blacks are considered to be in high-risk for prostate cancer as well as those who have first or second degree relatives who had prostate cancer at a young age (<55 years).
Can prostate cancer be prevented?
Dietary habits appear to play an important role in the appearance of clinical cancer which is favored by the consumption of fatty foods and red meat. In contrast, fruits, vegetables, soybeans and foods containing phytoestrogens appear to act prophylactically. There is evidence from studies which indirectly indicate that vitamin E, selenium, lycopene (contained in tomatoes) decrease the incidence of prostate cancer, whereas a large randomized chemoprevention study showed that finasteride (medicine given for symptomatic hyperplasia ) reduced the occurrence of prostate cancer by 25%.
What are the symptoms of prostate cancer?
Early prostate cancer may not have any symptoms and it is important that it is diagnosed through other techniques that will be explained below. If symptoms of dysuria grow very quickly, this may be a symptom of prostate cancer, although most men with symptoms of dysuria do not have prostate cancer. Some patients have only general symptoms such as weakness, anorexia, weight loss or pain at the waist that is usually due to dispersion of the disease in other parts of the body.
What is needed to make the diagnosis?
Digital rectal examination
The simplest and also necessary examination is the digital rectal palpation of the prostate from the rectum. When cancer is present, the prostate feels hard, this does not necessarily mean that induration of the prostate is a sure sign of cancer. In the early stages of prostate cancer, digital rectal examination may yield normal results.
Prostate specific antigen (PSA)
PSA is a special protein produced in the prostate gland and is needed for sperm liquidation. When the gland architecture is disrupted (as it happens in the case of cancer) small amounts escape into the blood circulation where they can be measured. Small or moderate elevations in the blood circulation often accompany benign conditions such as BPH or prostatitis. Thus, an increase in PSA does not always mean that prostate cancer is present, but of course a urologist consultation is required.
Transrectal ultrasound
If an increased PSA value is found, or if there is an abnormality during the digital rectal test, the next examination is the transrectal ultrasound (TRUS). It is a simple test that lasts 1-5 minutes and requires no anesthesia The transrectal ultrasound provides useful information that guides the following biopsies of the prostate.
Biopsy of the prostate gland
It is the final examination that provides the concluding diagnosis. Usually it is made through the rectum by means of transrectal ultrasonography. It is simple and requires no anesthetic. Several pieces of the prostate gland are extracted and given to the pathoanatomist who provides the histological diagnosis.
How is prostate cancer treated?
The type of treatment depends on the stage (extent of the disease), age of the patient, the general health condition and his preference. It should be noted that prostate cancer is a slowly progressive disease and when it is usually detected in old age, it is not terminal because the patient is dying from another cause. This means that not all men with prostate cancer are in need of urgent treatment. For younger patients (<75) the treatment is necessary because if every man lives long enough he will eventually die of prostate cancer.
a.Treatment of localized prostate cancer:
If a cancer is localized only in the prostate gland, it can be treated in various ways, by simply monitoring the well differentiated tumors in aged patients by radical local therapies aimed at curing the patient including radical prostatectomy and radiotherapeutic methods.
Radical Prostatectomy is the surgery in which the entire prostate gland along with the capsule and the seminal vesicles are removed while the urethra is reconnected to the bladder. In the past, it was usually accompanied by high rates of urinary incontinence and impotence. Today, however, these percentages are much smaller.
Radiation therapy: This involves the use of high energy X-rays that kill cancer cells. Radiation therapy may be external or internal by implanting radioactive seeds in the prostate (brachytherapy).
b. Treatment of advanced prostate cancer
When cancer has spread from the prostate gland to other parts of the body such as the lymph nodes or bones, it can still be treated with good remission rates but it cannot be cured. It is treated by hormonal therapy whose aim is to deprive the prostate of male hormones. When cancer becomes resistant to hormonal therapy, second-line hormonal treatment can be used involving drugs that affect bone metabolism and chemotherapy.
Recommendations
Because prostate cancer is cured during its the early stages, the main goal is early detection. Unfortunately, in the early stages there are no symptoms so that a patient may decide to visit a doctor.
For this reason:
• Every man over the age of 50 should be tested annually for prostate cancer.
• People who have first or second degree relatives who developed prostate cancer at an early age should begin testing at an earlier age (40).
• Avoiding fatty foods and red meat as well as a frequent consumption of vegetables and fruits protect against prostate cancer.
Prostatitis (inflammation of the prostate gland)
Sometimes the prostate gland swells from inflammation, called prostatitis. Prostatitis is the most common urological disease in young males (up to 50) and the third most common urological disease in elderly men (after benign hyperplasia and prostate cancer). Among adults, 50% will display symptoms of prostatitis at some point in their lives.
The symptoms that accompany this condition can last for a long time and be very distracting.
Prostatitis includes conditions such as dysfunction of the lower urinary tract and pelvic floor muscle aches, conditions in which evidence of inflammation is not present.
Approximately in 5-10% of cases, prostatitis has a proven microbial etiology (acute and chronic bacterial prostatitis). In the remaining 90%, the laboratory methods fail to identify pathogens and these patients are classified in the category of chronic pelvic pain syndrome.
The various forms of prostatitis are classified as follows:
• Category I: Acute bacterial prostatitis
• Category II: Chronic or recurrent bacterial prostatitis
• Category III: Chronic pelvic pain syndrome (CP/CPPS)
• Subcategory IIIA: Inflammatory CP/CPPS
• Subcategory IIIB: Non-inflammatory CP/CPPS
• Category IV: Asymptomatic inflammatory prostatitis
Acute and chronic bacterial prostatitis are well defined inflammatory diseases of the genitourinary system. The most common microorganisms are the Gram negative (particularly the E.Coli, 60-80% of cases).
Acute prostatitis is characterized by high fever, chills, high urinary frequency, dysuria, urinary obstruction in varying degrees, nocturia, pyuria, hematuria, pain in the perineal area and back pain (often accompanied by myalgia and arthralgia). The gland is diffusely hyperemic, swollen and sensitive to palpation. It is treated by using antibiotics. If not fully cured, it switches to chronic inflammation characterized by discomfort in urination, pain in the perineum, the suprapubic region and sometimes pain during ejaculation. The discovery of the responsible microbe is achieved by examination of the prostatic fluid after prostatic massage, although sometimes it may be also achieved by sperm culture which is not as reliable. It is usually treated by the use of long-term antibiotics.
Similar symptoms can exist in the absence of germs in the prostatic fluid (except pyuria and/or without any evidence of inflammation).
In such cases (chronic pelvic pain syndrome), the etiology, pathogenesis and pathophysiology is unknown. The mechanisms that seem to be involved in the etiology and pathogenesis of chronic pelvic pain syndrome are:
• Microorganisms
• High-pressure urination due to blockage (neck bladder, urethral stricture, outer sphincter contraction) or dysfunctional urination
• Intraprostatic reflux of urine
• Cytokines-autoimmune mechanisms
• Chemically induced inflammation
• Neuromuscular disorders
• Psychological factors
Following administration of antibiotics, the treatment is more empirical, and many drugs have been tried but with limited results. Sometimes inflammation of the prostate may be an accidental finding during prostatectomy performed for gland hyperplasia.
Although inflammation has been implicated as a mechanism in the development of hyperplasia and prostate cancer, there is currently no strong scientific evidence to support this association.